AMIS Plus History
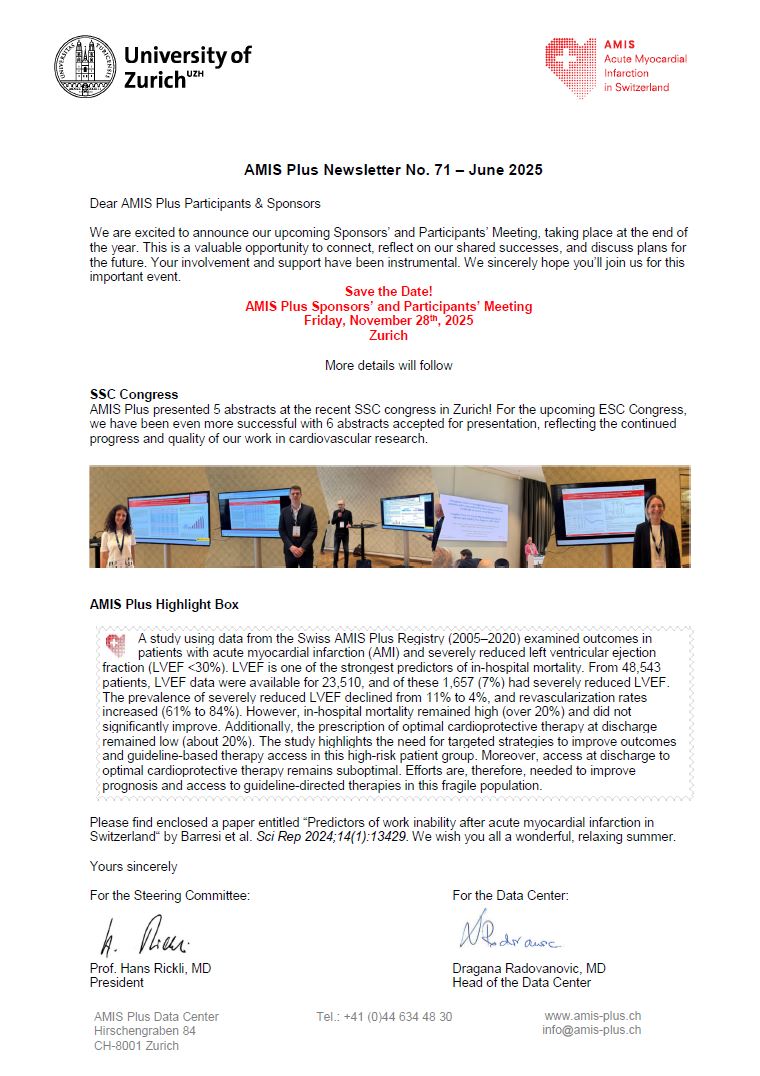
The AMIS (Acute Myocardial Infarction in Switzerland) project was initiated by a Steering Committee comprising representatives from the Swiss Societies of Cardiology, Intensive care and Internal Medicine. The AMIS Data Center was set up in 1997 by the Clinical Epidemiology Division of the Geneva University Hospital. In January 2000, unstable angina (UA) cases were included and AMIS was renamed AMIS Plus. In November 2000, the Data Center was transferred to the Institute of Social and Preventive Medicine (now Epidemiology, Biostatistics and Prevention Institute) of the University of Zurich and since March 2005, 12-month follow-ups are carried out. At the AMIS Plus Steering Committee Meeting on February 24, 2011, it was decided that inclusion criteria for enrollment in the registry should be restricted to acute myocardial infarction (STEMI/NSTEMI) and no longer include unstable angina. Unstable angina patients were underrepresented due to the limited resources available in participating hospitals.
Purpose of AMIS Plus
The AMIS Plus project has two main goals:
- To Maintain a Nationwide Registry
- An ongoing nationwide registry (database) of acute myocardial infarction
- Description of the patient population with acute myocardial infarction
- Description of treatment and hospitalization
- Description of outcomes 12-months after admission for acute myocardial infarction
- Epidemiological studies, e.g. definition of risk factors of patients with acute myocardial infarction, hospital mortality, time and cost-effective strategies as well as outcome measures
- Quality Control
- Evaluation of compliance with guidelines for the medical care of acute myocardial infarction
- Internal quality control through regular feedback and benchmarking
Methods
All Swiss hospitals admitting patients with acute myocardial infarction are eligible. Data are collected on demographics, risk factors, symptoms, laboratory results, invasive therapy, complications and medication.
Since the start in January 1997, the method of data collection has continuously improved in order to suit the different needs and technological advancements of the participating hospitals. Participants can either complete paper questionnaires and send them directly to the AMIS Plus Data Center at the Epidemiology, Biostatistics and Prevention Institute in Zurich where these questionnaires are then checked and entered online, or they can enter data directly online (AMIS online questionnaire). Data security is of high priority. Participant identification (code for hospital and physician) and a password are required to access the data entry form and send data.
Inclusion criteria
- Patients who had symptoms within the last 48 hours at hospital admission with a discharge clinical diagnosis of acute myocardial infarction or
- Patients who suffered an acute myocardial infarction in hospital during a hospitalization for other reasons
All patients with initial suspicion of acute myocardial infarction at hospital admission regardless of admission mode (emergency room, cathlab, intensive care unit, another ward) should be considered for inclusion in the AMIS Plus registry.
Acute myocardial infarction definition:
- Characteristic ischemic symptoms.
- ECG changes indicating new ischemia (ST-T changes or new left bundle branch block) or developing pathological Q-waves.
- A dynamic increase or decrease in biomarker or troponin (I or T) levels above the individual hospital cutoff for MI. The internationally accepted guidelines for troponin levels are set at least one value above the 99th percentile of the upper reference limit (URL).
Cut-off levels for either total creatine kinase (CK) or creatine kinase MB fraction (CK-MB) at least twice the upper limit of normal.
Patients can also be categorized as having ST-segment elevation MI (STEMI) or non-STEMI (NSTEMI) based on initial ECG findings:
- STEMI includes evidence of clinical and laboratory findings as described above and ST-segment elevation and/or new left bundle branch block on the initial ECG.
- NSTEMI includes patients with ischemic symptoms, ST-segment depression or T-wave abnormalities in the absence of ST-elevation on the initial ECG.